Juggling the physician and hospital side of revenue integrity
For one chargemaster analyst, a typical workday revolves around maintaining compliance for two different systems: the hospital chargemaster and the Medicare Physician Fee Schedule (MPFS). The chargemaster is built upon an automated system which utilizes work queues.
“On the hospital side, there’s so much more to consider,” says Nancy Woods, chargemaster analyst at Norton Healthcare in Louisville, Kentucky. “You have to make sure you’ve got the correct CPT® code. You have to check annually to make sure that’s not deleted and do you have the replacement. Do you have the right revenue code with the CDM or item or procedure? And have you included the right HCPCs code that goes with this revenue code.”
Norton Healthcare devised the CDM Request System, an in-house system that allows users to add procedure and supply requests in an automated process. It’s ideal for adding, changing or deactivating/reactivating a CDM, says Woods.
When a supply request is submitted through the system, the form is automatically sent to materials management for review. Next, the form is passed along to Woods to ensure that all fields have been completed accurately. Once approved, the data goes to information services (IS), which receives requests in a work queue. Procedure requests follow the same process, although these are sent directly to Woods rather than to materials management.
“The next morning our EPIC IS person uploads all the requests into EPIC. It’s then available to the users later that day or the next day,” says Woods. “It’s just a really good way of getting the data into EPIC, and providing a history of all requests submitted.”
The process is constantly reviewed and upgraded. In 2017, one such upgrade included the addition of a modifier field in the CDM Request form. Woods worked with her IS team to make the addition. This gives Woods the ability to pull reports regarding modifiers being used.
Another success has been educating department managers on using the CDM Request System, says Woods. Managers generally make requests through email, but there isn’t always enough information provided to make the update. Woods and/or a revenue integrity manager would then have to take the extra step of researching to channel back to the reasoning behind the CDM request and the appropriate data needed to complete it.
For 2018, Woods hopes to get all departments on board with using the CDM Request System. She and a revenue integrity manager are assessing the reasoning behind the lack of system usage. They are also working on an education strategy, a process that involves establishing a comprehensive list of staff members in each department and identifying who will be the appropriate contact for submitting requests and addressing questions.
On the other side of Woods’s workflow is managing the MPFS, a list of Medicare fees for physician reimbursement. These include Medicare established CPT and HCPCS codes, descriptions and prices charged on the bills.
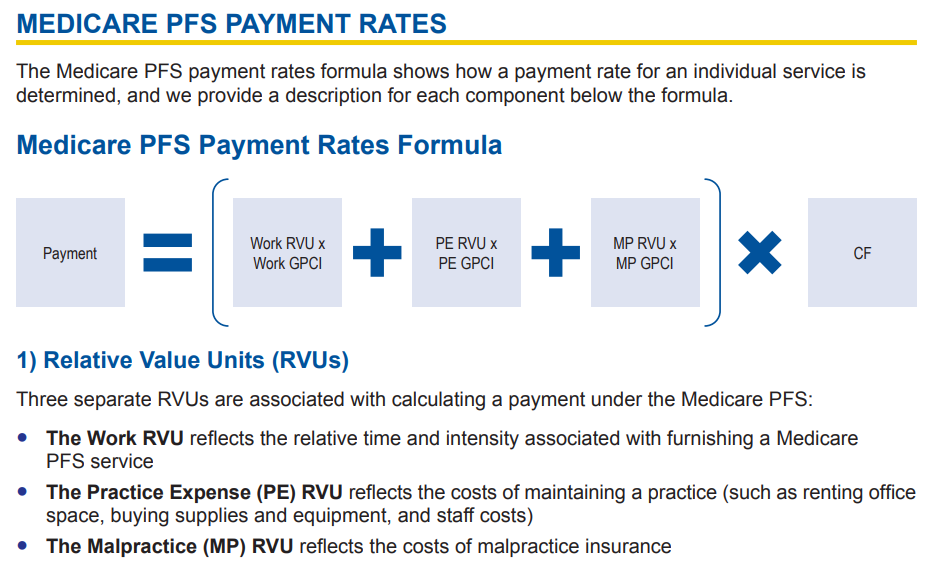
The MPFS payment rate is determined by relative value units (RVU), geographic practice cost indices (GPCI), and the conversion factor (CF), explains MLN Matters in its Medicare Physician Fee Schedule Fact Sheet.

According to Woods, Norton Healthcare physician services has several different fee schedules, from facility based to non-facility based. One example is the occupational medicine fee schedule, which is broken down into a client fee schedule and a worker’s compensation schedule.
The challenge then, is assessing how to manage the MPFS. “I’m trying to come up with a way to have a request system that staff can use when they need to add a new code, or make changes to an existing code, rather than just sending an email and saying hey, we need this new code or need to make this change,” says Woods.
In 2018, she (with IS help) hopes to develop a system like the CDM Request System to queue up CPT/HCPCS code requests. Developing this type of system would improve workflow, automate the process, and provide a history of requests submitted, says Woods.
The other challenge of fee schedules is monitoring the pricing and the CPT codes. While the MPFS isn’t as nuanced as the hospital chargemaster maintenance, it still needs monitoring to ensure compliance. This involves annually reviewing the MPFS on the CMS website. The CY 2018 Medicare Physician Fee Schedule Final Rule, released November 2, 2017, denotes new policies and codes, deleted codes, and replacement codes.
Woods recommends utilizing reports and audits to ensure that the pricing matches what’s in your system.
For more information on using the MPFS, see the MLN Booklet How to Use the Searchable Medicare Physician Fee Schedule.